Intro
Improving population health has become a strategic goal for healthcare organizations, but achieving it requires more than expanded programs or better outreach. It requires a clear understanding of what is happening across patient populations and why. That level of clarity only comes from using data in the right way.
Most healthcare systems already collect vast amounts of data from electronic health records, claims, labs, and community health programs. But raw data alone does not translate into better outcomes. The challenge lies in connecting those scattered data points, analyzing them meaningfully, and turning the insights into coordinated action.
This blog explores how healthcare providers and payers can use data analytics to improve health outcomes across populations. From integrating multiple data sources to designing targeted interventions and measuring results, the goal is to shift from broad assumptions to precise, data-informed strategies that actually change how care is delivered.
Building the Data Foundation
A strong data foundation supports not only analytics, but also broader population health management frameworks that connect clinical data, community health insights, and coordinated interventions.
- Data integration from multiple sources
Combining data from EHRs, claims, lab systems, SDOH, wearables, and patient surveys provides a comprehensive view of patient health. Social determinants such as housing, income, and food access add layers of context missing from clinical data alone. - Interoperability through standards
Adopting standards like HL7 or FHIR allows systems to exchange data consistently. Frameworks like DHIS2 already support these standards and enable platforms to aggregate wide-ranging health data. - Data quality and governance
Clean, complete data is non-negotiable. Organizations must enforce quality controls and monitor missing or inconsistent values. Governance layers must enforce HIPAA-compliant access, consent tracking, and auditing to ensure trust in analytics. - Privacy and compliance safeguards
To use healthcare data effectively, organizations must align with privacy regulations and patient consent models. This ensures analytics remain ethical and legally grounded.
This data foundation ensures analytics operate on accurate and meaningful inputs, enabling better segmentation, risk prediction, and outcome tracking.
Apply Analytics to Identify Risk and Opportunities
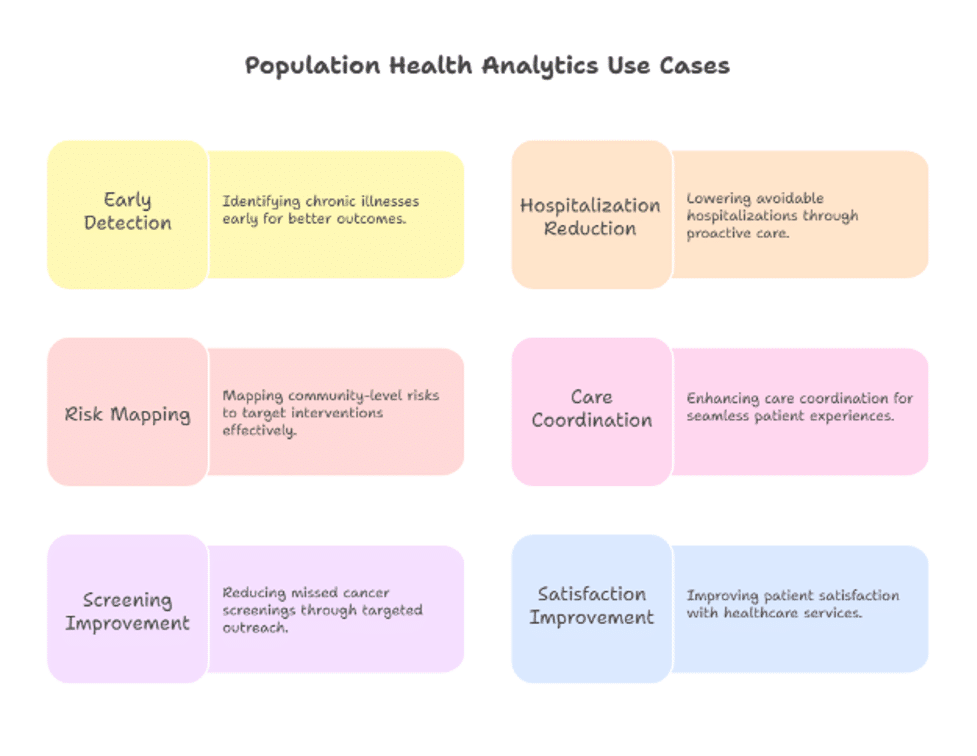
With integrated and trustworthy data in place, analytics can uncover population insights and highlight where action is needed:
- Risk stratification
Tools segment patients into groups such as high-risk, high-cost cohorts using clinical and social data. These tools help prioritize outreach and resource allocation. A recent review found many primary care systems using risk stratification to reduce utilization and improve chronic care outcomes. - Predictive modeling
Machine learning can forecast conditions such as kidney failure, readmissions, or frequent ER use. Models like those used in Boston hospitals for chronic disease prediction achieved high accuracy while remaining interpretable for clinicians. - Analyzing social determinants of health
Including SDOH data significantly improves predictive models’ accuracy and fairness. In one study, models combining clinical and social data performed more effectively and highlighted deeper drivers of poor outcomes. - Role of AI and automation
AI tools can detect patterns and flag issues earlier. For example, models built from multiple inputs, clinical and behavioral, can raise early alerts for deteriorating kidney function or rising risk of acute hospitalization.
Example: In a Medicaid cohort, predictive analytics identified early-stage kidney disease in a subset of patients. Interventions like care management and tailored treatment lowered hospitalization rates and slowed disease progression.
Design Interventions That Make the Data Actionable
Once risk groups are identified, the real work begins turning insights into action. Effective population health management depends on converting analytics outputs into targeted interventions that can be tracked, refined, and scaled.
- Coordinated care with shared dashboards
Care coordination is easier when teams operate from the same information. Shared dashboards give care managers, primary providers, and behavioral health teams a unified view of a patient’s clinical status, social needs, and outreach history. For instance, some health systems use interactive care management tools to flag patients with overlapping needs such as housing insecurity and medication nonadherence and coordinate follow-up accordingly. - Personalized interventions
Patients with the same diagnosis often require very different care pathways. Analytics helps segment not just by disease, but by behavior patterns, socioeconomic status, and comorbidities. A patient flagged for high diabetes risk may benefit from text-based coaching, while another needs a referral to a local food access program. Personalizing the mode and content of intervention can dramatically improve engagement. - Community-driven outreach
Aggregated data at a geographic level reveals trends that inform broader public health action. For example, if a dashboard shows a specific zip code has low cancer screening uptake, it may prompt mobile screening units, education campaigns, or partnerships with community organizations. - Preventive care gap closure
Many health systems use analytics to identify patients overdue for preventive services. These systems can automate alerts or send reminders, significantly improving compliance with screenings, immunizations, and annual wellness checks. Reducing these gaps helps catch diseases earlier and lowers long-term care costs.
The key is using it to match the right action with the right individual or community needs at the right time.
Measure What Matters and Continuously Improve
No population health strategy is complete without measurement. But the right metrics and ongoing evaluation are what separates sustainable impact from one-time efforts.
- Defining the right KPIs
Metrics should reflect clinical, financial, and operational outcomes. These include hospitalization rates, 30-day readmissions, ER utilization, care plan adherence, and the ROI of specific programs. Just as important are patient-reported outcomes and satisfaction scores. - Dashboards for decision-makers
While frontline staff need granular patient views, leadership needs aggregated trends to guide resourcing and strategic investments. Visual, role-specific dashboards allow clinicians, care managers, and executives to focus on what matters most to them. - Establishing a feedback loop
Population health analytics must evolve. Interventions that worked last year may no longer be effective. Successful programs use regular data reviews to refine targeting, messaging, and resource allocation. This loop is essential to maintaining relevance in dynamic healthcare environments.
Example: One state Medicaid program used quarterly data reviews to assess diabetes prevention initiative. While initial outreach rates were strong, analysis showed engagement was lower in rural areas. By introducing peer health educators from the community, participation nearly doubled the next quarter demonstrating how iterative improvements can dramatically boost outcomes.
Continuous measurement ensures that population health strategies do not stall. They mature with data, adapt to shifting needs, and deliver better outcomes over time.
Best Practices for Scaling Population Health Analytics
Early wins in population health analytics often come from pilot programs or narrowly scoped initiatives. But to drive system-wide change, organizations need to move from one-off projects to scalable, repeatable strategies supported by strong foundations.
- Invest in infrastructure and skilled analysts
Scalable analytics demands a robust data platform, scalable storage, real-time processing capabilities, and secure access controls. Equally important is a multidisciplinary team that can interpret data through both clinical and operational lenses. Health systems are increasingly hiring clinical informaticists and data scientists who can bridge the gap between numbers and actions. - Foster a culture of data-driven decision-making
Scaling requires more than dashboards. Clinicians, administrators, and outreach staff need to trust and understand how data informs decisions. This involves not only training but also showing how analytics improves outcomes and reduces friction in everyday workflows. - Collaboration across departments and community partners
Silos remains a major barrier. Effective population health initiatives require coordination between providers, social workers, public health agencies, and community organizations. Data-sharing agreements and joint-governance models help ensure interventions are comprehensive and sustainable. - Address ethical concerns head-on
As analytics programs scale, so do concerns about bias, transparency, and patient consent. Building trust means going beyond compliance. Organizations must implement clear governance frameworks, ensure explainability of AI models, and establish processes for patient feedback and accountability.
Scalability is not just about technology, it’s about alignment. The most successful organizations are those that align people, processes, and data to create a learning health system that continuously adapts to serve populations better.
Conclusion
Improving population health is about using it wisely. As this guide has shown, the path from data to better outcomes requires more than dashboards and reports. It takes integrated systems, predictive insight, targeted interventions, and a culture of continuous improvement.
Healthcare organizations that invest in the right analytics foundation can identify risk earlier, coordinate care more effectively, and design interventions that actually move the needle. But making this shift at scale requires the right technology, team, and governance.
For providers and public health networks ready to operationalize this vision, partnering with experts in healthcare data analytics services can accelerate impact. Whether it’s building a population health dashboard, designing predictive models, or supporting data integration, the right guidance ensures analytics becomes a driver of health equity and smarter care.